Patient compliance strategies that actually work in physiotherapy
Key Takeaways
- Patient compliance in physiotherapy means following agreed treatment plans both in clinic sessions and through home exercises consistently
- Digital tools work best when they support rather than replace human contact with supervised exercise, showing four times higher adherence rates
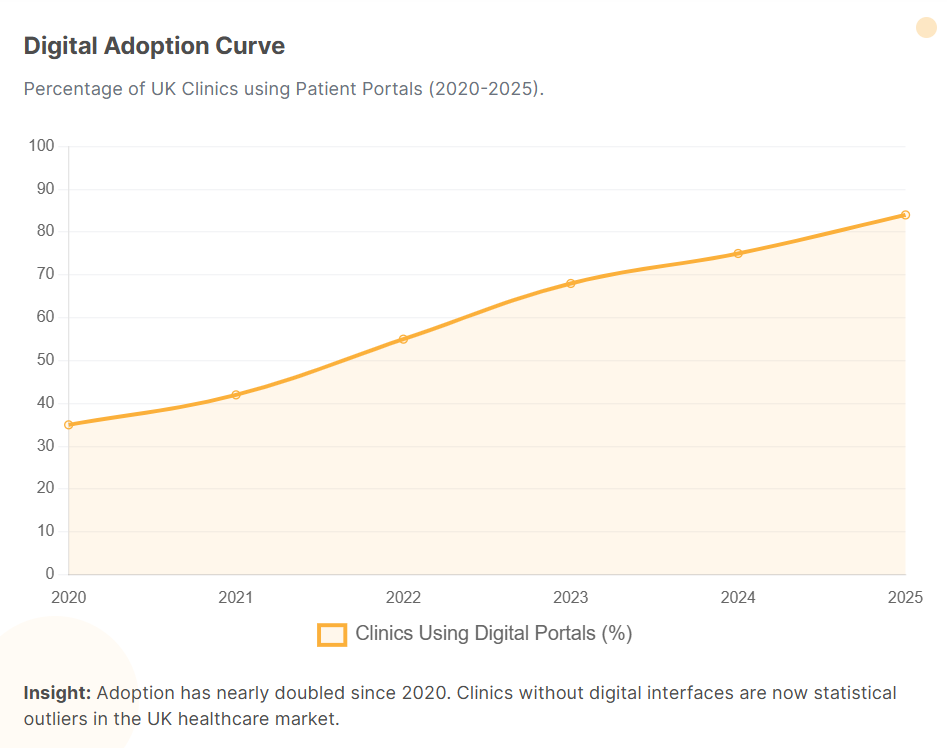
- Practice management software reduces missed appointments by automating reminders and making booking friction-free for patients
Many physiotherapy patients start treatment with good intentions, but struggle to follow through with home exercises and appointments. Research confirms this challenge, showing that only 53.7% of patients fully comply with their post-operative physiotherapy programmes. The result? Slower recovery, more setbacks, and treatment plans that never quite deliver.
This article explains what patient adherence means in physiotherapy, why it directly affects clinical outcomes, and which practical strategies help physiotherapy teams support better follow-through.
What is patient compliance in physiotherapy?
Patient compliance in physiotherapy is the extent to which someone follows the therapeutic regimen agreed with their physiotherapist, in the clinic and at home. It includes attending physiotherapy appointments regularly, performing home exercises at the recommended frequency, using correct technique, and following simple advice on pacing, posture, and activity levels. You may also see adherence or concordance used, but all three terms point to the same idea: patient and physiotherapist working together so plans are followed consistently and safely.
Why patient adherence matters for physiotherapy outcomes
Adherence is a key factor in how effective physiotherapy will be. When patients follow their programme, the work done in sessions and at home builds on itself instead of restarting after every gap.
Good adherence can:
- Make treatment more effective, because exercises are carried out as intended
- Support smoother recovery, with fewer setbacks from missed sessions
- Give healthcare professionals clearer information for adjusting programmes
Poor adherence, on the other hand, is linked with worsening symptoms, more flare-ups, and longer treatment journeys. Keeping adherence at the centre of assessment and planning helps physiotherapists design programmes that patients can realistically sustain in daily life. A well-structured patient management system can also support this by making it easier to coordinate care and monitor progress.
Common reasons for poor patient compliance
Poor patient compliance rarely has a single cause. It usually reflects a mix of beliefs, programme design, practical issues, and system-level factors.
Patient and belief-related factors
Barriers include doubt that exercises will help, worry about pain, anxiety, low mood, and forgetfulness. Social and cultural influences can further shape how seriously patients take medical advice.
Studies confirm that psychological factors significantly impact adherence. Patients with higher self-efficacy are more than three times as likely to stick with their programmes, while high fatigue show notably lower compliance rates. Understanding these risk factors helps healthcare providers design more effective support strategies.
Treatment and communication-related factors
Problems often arise when programmes include more exercises than patients can manage, instructions are unclear, or exercises feel too painful. Understanding and addressing these barriers early in treatment helps physiotherapists design programmes that patients can realistically follow.
Practical and system-related barriers
Cost, travel, appointment clashes with work, and limited home space all make it harder to stick with a plan. Short appointments with little time for questions and weak reminder systems leave patients feeling unsupported. Primary care and physiotherapy services that align workflows with clear practice management standards provide a more consistent experience.
How to improve patient compliance: Practical strategies
Improving patient compliance comes from a mix of clear communication, personalised planning, patient education, and steady support. Healthcare professionals who combine these with simple behaviour change techniques usually see more consistent follow-through.
1. Build trust and a supportive relationship
Patients are more likely to stick with their plan when they feel safe, heard, and respected. Patience experiences typically show that when people find acceptable, scientific explanations for their pain, they describe the experience as empowering, transforming them from victims of a condition to active managers of it.
Tips for clinicians:
- Start by asking how things have been since the last appointment
- Treat lapses as shared problems to solve, not failures
2. Communicate clearly and educate with purpose
Patients need to understand both what to do and why it matters. Using plain language and linking exercises to specific problems makes the programme more meaningful. Effective patient education builds confidence and improves clinical outcomes.
Pain neuroscience education has proven particularly effective. When patients understand the science behind their pain rather than fearing movement will cause harm, adherence rates can reach 81 to 100% in some patient groups.
Tips for clinicians:
- Replace clinical terms with everyday language wherever possible
- Ask patients to demonstrate and explain the plan back in their own words
3. Tailor programmes and goals to real life
Programmes that fit around real schedules and environments are easier to maintain. Patients are more likely to comply when they help choose exercises and feel the overall load is realistic.
Tips for clinicians:
- Ask when and where exercises can realistically happen in a normal week
- Set one or two short-term goals linked to meaningful daily activities
4. Use behaviour techniques in daily routines
Simple behaviour strategies make exercises easier to remember and start. Planning prompts, habit stacking, and pairing exercises with enjoyable activities all help turn intention into action.
Tips for clinicians:
- Agree on a specific plan, such as "after breakfast, I do my first set of exercises."
- Suggest linking exercises to existing habits, like making tea or watching evening television
5. Use digital tools for reminders and tracking
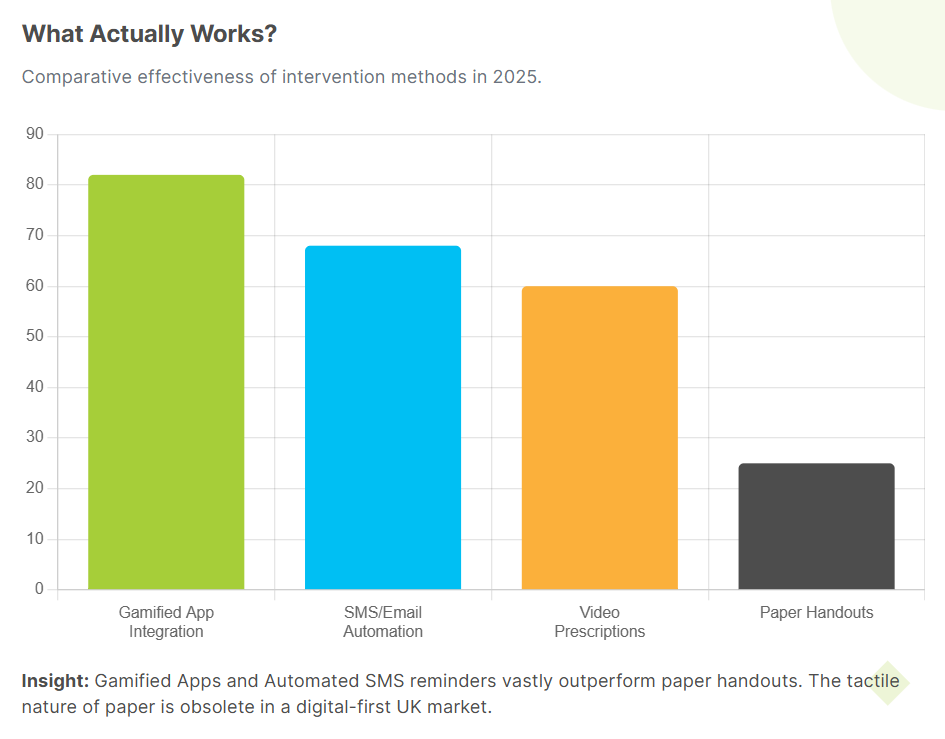
Digital health tools can support compliance without adding extra work for clinicians. Remote monitoring through apps can catch problems early before they derail a programme.
Digital tools work best when they support rather than replace human contact. Supervised exercise typically produces adherence rates more than four times higher than app-only approaches, making blended care the most effective model.
Tips for clinicians:
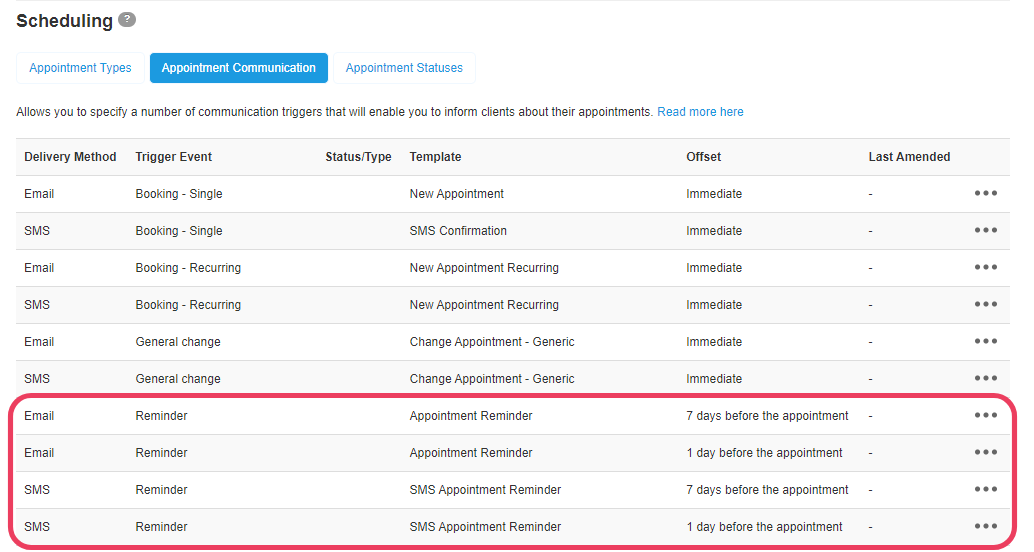
- Use practice management software to send appointment and exercise reminders by SMS or email
- Share home exercise programmes that patients can view on their phone or computer
If your clinic is reviewing its software, it is worth checking whether your system includes the key features of a patient management system that support communication, reminders, and record keeping.
Impact of PMS Features on Compliance Metrics
PMS Feature
Mechanism of Action
Evidence of Impact
Automated Reminders
Sends SMS/Email prompts 24-48 hours pre-appointment. Removes "forgetting" as a cause for DNA.
A physiotherapy practice reduced DNAs by over 30% in two months.
Online Booking
Allows patients to book/reschedule at their convenience (24/7). Increases patient agency and reduces admin friction.
Saved 10+ hours of admin per week; filled 25% more appointment gaps.
Smart Forms
Pre-visit assessments sent digitally. Patients tell their story before arrival, improving data accuracy and engagement.
Improves accuracy; speeds up check-in; ensures clinicians are prepared.
Integrated Payments
Captures payment or card details at booking. Creates a financial commitment to the slot.
Significantly cuts down on no-shows by monetizing the reservation.
6. Maintain feedback, follow up, and positive reinforcement
Ongoing contact helps patients stay on track and feel supported. Regular reviews are a chance to adjust the plan, address barriers, and highlight progress that patients may not notice themselves.
Tips for clinicians:
- Use each review to point out at least one clear area of progress
- When treatment plan adherence drops, ask what got in the way before changing the plan
7. Involve support networks when helpful
Family members or carers can make it easier for some patients to follow their plan. When the right person understands the goals and how to help, they can remind, encourage, and sometimes assist with exercises.
Tips for clinicians:
- Ask if there is someone the patient trusts who could support exercises at home
- Invite that person to key sessions where you explain and demonstrate the plan
What about patient compliance with medication?
Many physiotherapy patients also manage chronic diseases and take medicines prescribed by primary care providers or specialists. How consistently they follow their medication regimen can directly influence their progress in physiotherapy. Patients with chronic pain who struggle with medication compliance may experience more severe symptoms that make exercise programmes harder to sustain.
Medication adherence challenges often mirror physiotherapy adherence barriers. Patients may forget doses, worry about side effects, or misunderstand instructions. Healthcare providers can support better medication compliance by reinforcing key messages from prescribers, asking patients about concerns or side effects that might affect exercise tolerance, and recording medication information in shared digital records. When medication regimens and physiotherapy plans are aligned and clearly communicated, patients achieve better clinical outcomes across both areas of care.
Support patient compliance with WriteUpp
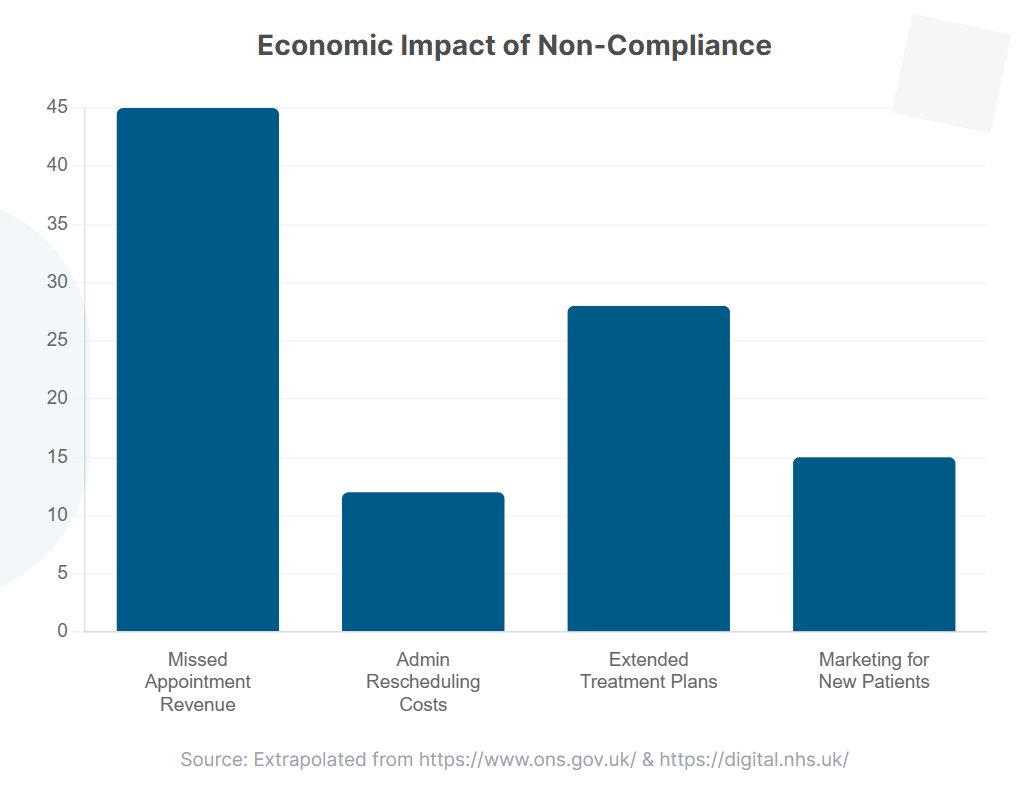
Missed appointments represent significant waste in healthcare systems. NHS data shows these losses extend beyond the immediate slot to include facility overhead, clinician time, and administrative costs, all without corresponding value generation.
WriteUpp gives physiotherapy teams simple tools that support compliance strategies:
- Online booking and payment processing: Patients book and manage appointments at any time, reducing friction around attending sessions.
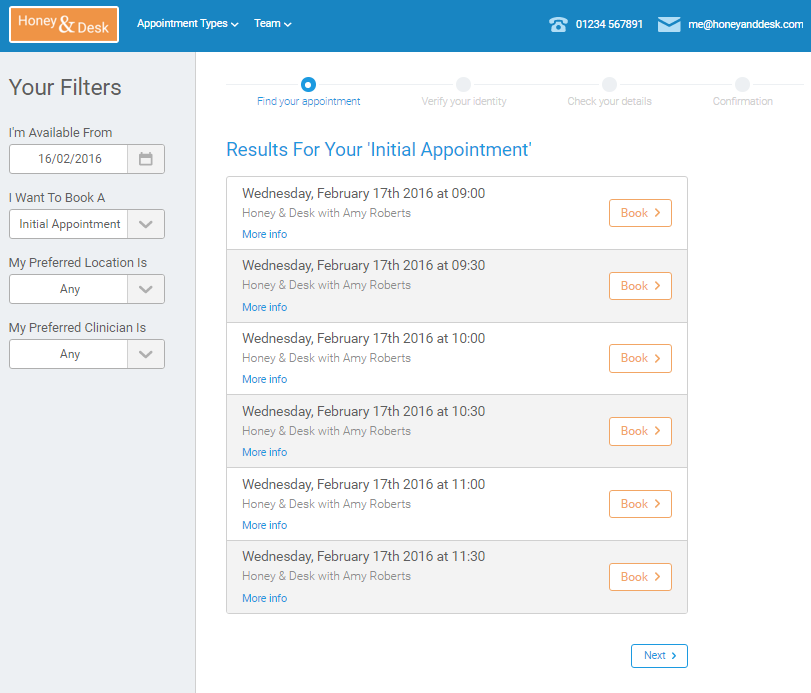
- Automated reminders: SMS and email reminders reduce missed or late-canceled appointments.
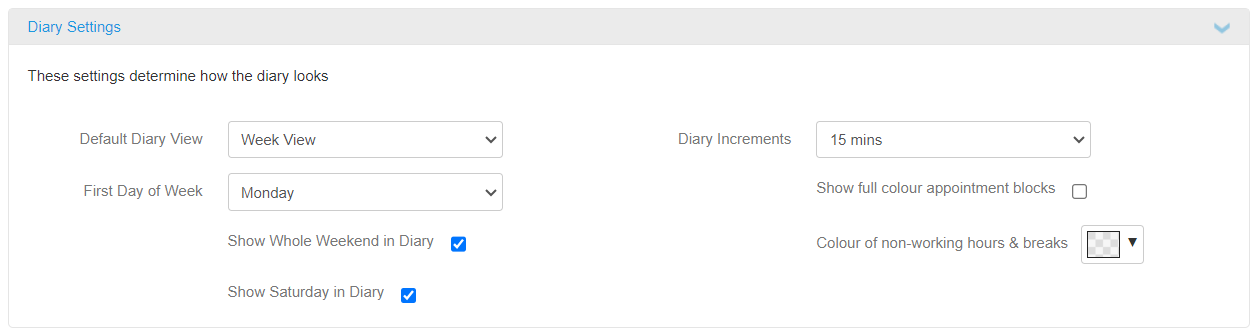
- Diary management system: Clinicians fill gaps quickly, keeping treatment plans moving with fewer long breaks.
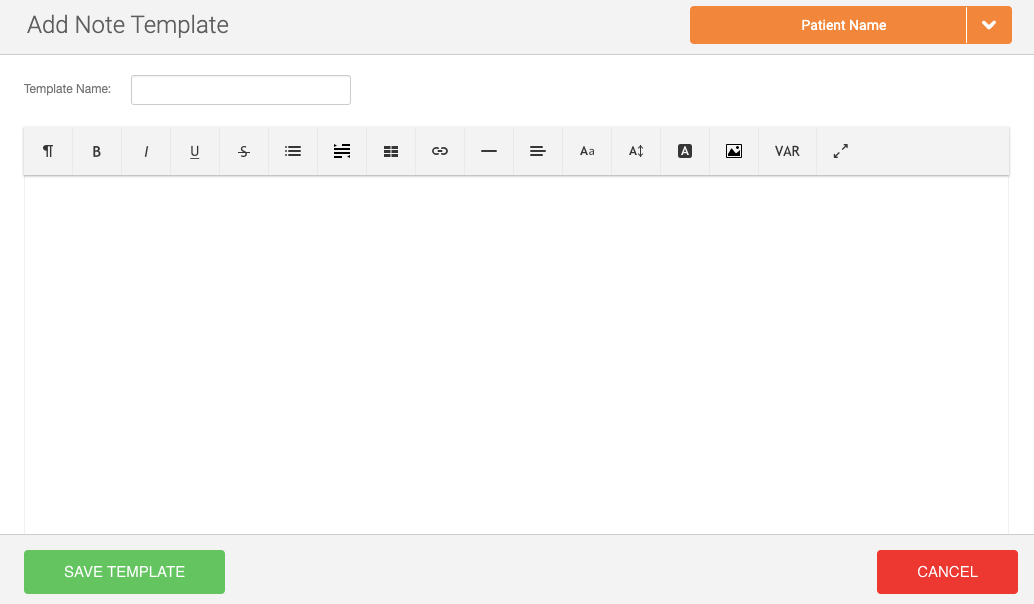
- Smart Forms: Digital forms capture information before sessions, so clinic time focuses on education and coaching.

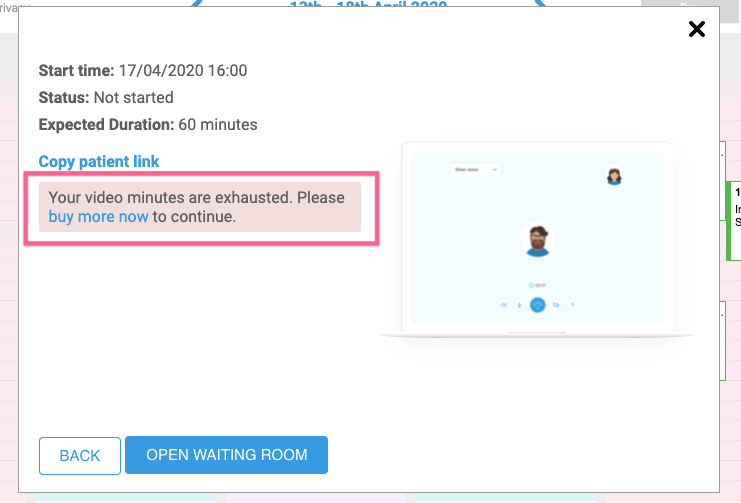
- Video consultations: Built-in video appointments within WriteUpp's clinic management software make it easier to continue treatment when patients cannot attend in person.
- Centralised notes: Track attendance, adherence, and progress in one secure place.
For healthcare professionals who want to strengthen patient compliance in a practical way, using WriteUpp as the hub for bookings, reminders, forms, and notes provides a strong foundation for better outcomes.
Final thoughts
Patient compliance reflects how well therapeutic regimens fit into real lives, how clearly goals are explained, and how practical it is for patients to follow through. By combining thoughtful communication, realistic programmes, and supportive technology, physiotherapy teams give patients every opportunity to stay on track.
If you want to make these strategies easier to deliver day to day, you can see how WriteUpp supports better patient compliance.



Join over 50,000 clinicians that we've helped using WriteUpp
Start my free trial




.png)

.png)

