Effective Patient Communication for Better Care Results
Key Takeaways
- Poor patient communication is a significant contributor to patient safety incidents and can lead to misunderstandings that affect care quality
- Patient-centered communication requires four core strategies, including clear language, active listening, showing empathy, and tailoring your approach to individual needs
- Common barriers like medical jargon, time constraints, and language differences create gaps that damage trust and reduce patient engagement
- Digital tools, including electronic patient portals, automated reminders, and video consultations, help clinics maintain consistent communication throughout the patient journey
- Strong physician-patient communication directly improves treatment adherence, patient satisfaction, and builds the therapeutic relationship needed for better outcomes
Patient communication shapes every part of the care experience. When conversations are unclear, rushed, or one-sided, patients leave appointments unsure about their next steps. They might misunderstand treatment plans, skip important follow-ups, or feel too uncertain to raise concerns that matter.
These gaps show up in ways clinicians recognize: repeat calls for clarification, patients arriving unprepared, concerns that were never raised, or treatment plans that weren't followed correctly. Poor communication directly impacts health outcomes and represents a significant contributor to patient safety incidents. Improving physician-patient communication helps minimize these frustrations and supports better outcomes.
This article outlines practical communication strategies to improve patient-clinician communication in daily clinical work and why these approaches contribute to better care results.
What is patient communication and why it matters
Patient communication is the exchange of information between a clinician and a patient in a way that supports understanding, comfort, and informed choices. It shapes how clearly patients understand their treatment plan, how confident they feel during appointments, and how engaged they stay throughout their patient journey.
Patient-centered care relies on plain language, active listening, and an awareness of each patient's needs. It reduces confusion, supports shared decision-making, and encourages patients to take an active role in their health. When conversations are respectful and tailored to the person in front of you, trust grows naturally, and the patient experience improves.
Core principles
Build trust
Give patients space to describe their concerns without interrupting. Respond in a calm, steady manner that shows you're paying attention. Provider-patient communication and trust are significant factors influencing shared decision-making, with trust acting as a key mediating factor.
Use clear language
Choose simple terms when explaining treatments or next steps. Break information into smaller points and provide quick examples when a concept feels complex.
Support shared decision-making
Outline the available options in a balanced way. Ask what matters most to the patient before finalizing a plan, and check patient comprehension by inviting them to summarize key points.
Take a patient-centred approach
Shape conversations around the patient's comfort level and preferences. Adjust the pace if they need more time and provide information in formats that match their needs.
Communicate respectfully
Recognize cultural and personal backgrounds that influence how people communicate. Use language that feels inclusive and create an environment where questions are welcomed.
Common barriers to communicating with patients
Communication challenges happen frequently across medical practice. Recognizing these barriers makes it easier to adapt your approach.
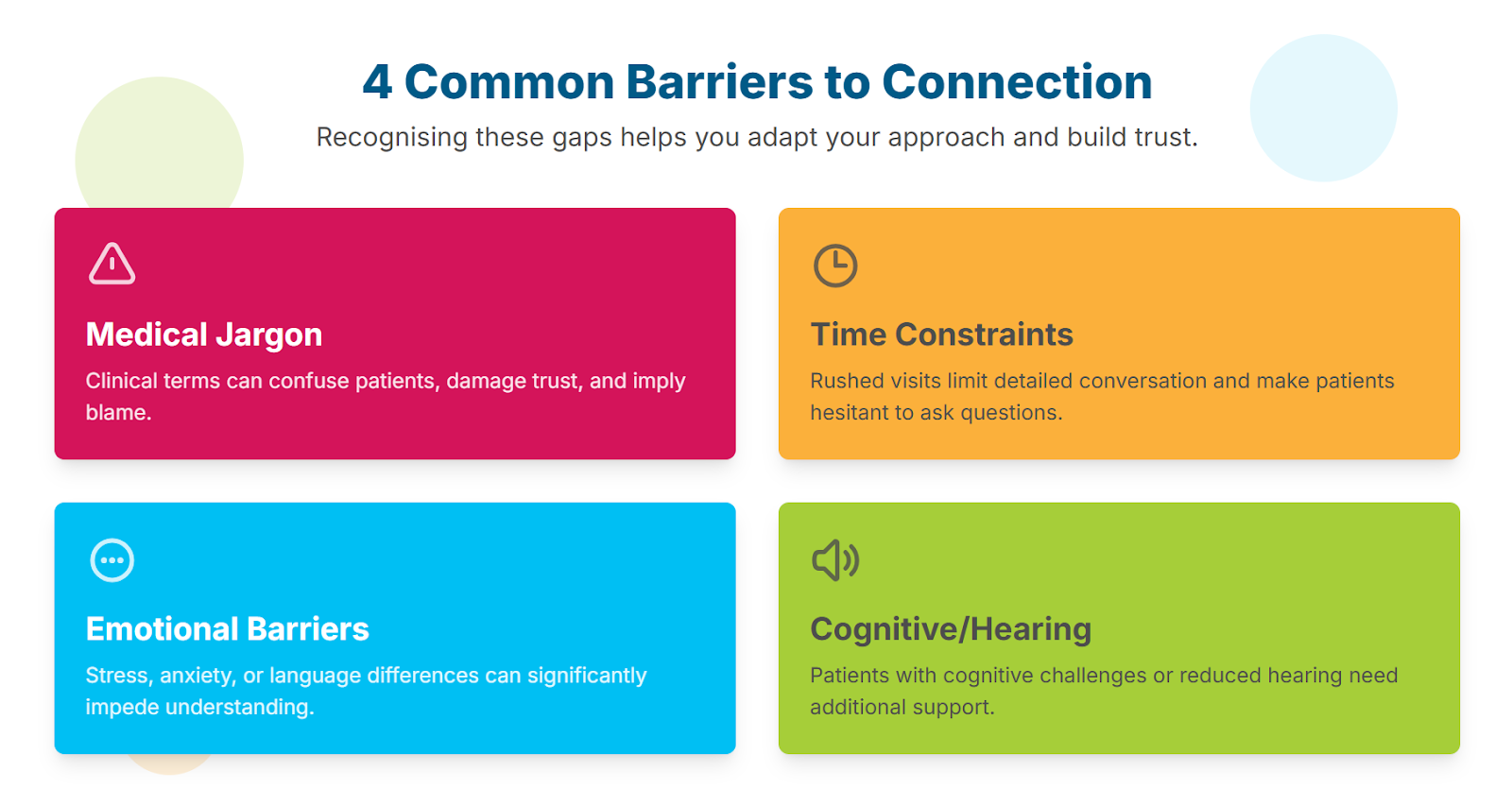
Medical jargon
Clinical terminology can confuse patients unfamiliar with it. The use of medical jargon has been shown to have a negative impact on patients and their health management, with language that can function as a barrier, undermining trust and patient understanding.
Time constraints
Busy schedules limit the time available for detailed face-to-face communication. Systemic pressures, where workload and time constraints, can inhibit optimal conversations that impact health outcomes. Patients may feel rushed or hesitant to ask follow-up questions.
Emotional or language barriers
Stress, anxiety, or cultural differences influence how patients interpret information. Language barriers contribute to unmet healthcare needs among families, affecting access to regular healthcare providers.
Cognitive or hearing impairments
Patients with cognitive challenges or reduced hearing need additional support. Communication problems have been shown to decrease the quality of care and triple the risk of preventable adverse events.
How to improve patient communication
Improving clinical communication requires clear language, empathy, and an ability to adapt your style to each individual. These communication strategies support stronger physician-patient communication.

1. Use clear and simple language
Patients process information better when explanations are direct and easy to follow. The use of simplified terms has been associated with better patient understanding and a greater sense of responsibility to take charge of health management.
Replace jargon with straightforward terms. Break information into smaller steps and provide clear patient instructions using short, simple sentences.
Avoiding medical jargon and confirming understanding through techniques such as teach-back and use of visual aids helps ameliorate potential risks associated with limited health literacy. Using the teach-back method promotes effective communication and enhances medication adherence and patient experience.
2. Practice active listening
Listening helps clinicians understand what a patient is trying to express beyond their words. This approach is key to making patients feel valued as partners in healthcare relationships.
Maintain eye contact where appropriate. Notice nonverbal messages through body language and facial expressions that may signal worry or confusion. Use simple acknowledgements to show attention and ask open-ended questions like "What concerns you most today?" to invite fuller responses. This improves face-to-face communication and patient satisfaction.
3. Show empathy and respect
Empathy strengthens physician-patient communication. New Canadian CLEAR guidelines recommend healthcare providers use active listening, empathy, compassion, and understanding toward the patient. Research on empathy in medical education defines empathy skills as including communication skills like active listening and avoiding jargon, alongside patient-centered care.
Use a calm tone. Acknowledge the patient's feelings and give space for questions. Empathy supports effective communication, producing positive effects such as increased emotional well-being and improved adherence.
4. Tailor communication to the individual
Every patient brings different patient communication needs and preferences. Tailoring your approach confirms that the information is understood clearly.
Adapt instructions for age, cultural background, or cognitive ability. Provide written visit summaries when needed and use visual aids to reinforce important points. This approach reduces barriers and confirms each patient receives information in a format that works for them.
5. Check understanding throughout the conversation
Confirming understanding prevents misunderstandings. Ask the patient to repeat key information in their own words. Invite questions before ending the appointment and provide visit summaries that patients can reference later.
6. Involve support systems when appropriate
Patients often benefit from having someone they trust involved in their care. Ask if they would like a family member included. Provide guidance that can be shared with their support system, which supports aftercare strategies for continued healing.
Benefits of strong patient communication
Improved patient-clinician communication offers several advantages that enhance the patient experience.
Better patient engagement
Patients who feel heard are more likely to participate actively. Good clinical communication encourages them to share concerns and understand their treatment plan. This creates a shared agenda between clinician and patient that improves patient experience.
Improved adherence and outcomes
Clear explanations help patients understand their condition. Poor communication is a primary reason for intentional non-adherence, with 68% of patients suggesting a follow-up call would improve adherence. Strong physician-patient communication supports better health outcomes.
Reduced misunderstandings and legal risk
When communication is consistent, there's less room for confusion. Patients who face language barriers are 30% more likely to experience harmful events during their hospital stay, highlighting the critical role communication plays in patient safety.
Enhanced patient satisfaction
Patients respond positively when they feel listened to. Virtual care programs in Canada report high patient satisfaction when communication is prioritized, contributing to stronger patient satisfaction overall. Regular patient feedback helps clinics identify areas for improvement.
Stronger therapeutic relationship
When patient-centered care is prioritized, trust grows naturally. Patients speak more honestly about their concerns, which helps clinicians provide better guidance and improves the overall patient experience.
Tools that help support better communication
Digital tools and electronic patient portals make it easier to keep patients informed throughout their patient journey. These communication tools help share updates quickly and create a smoother patient experience.
- Online booking systems: Online booking helps patients choose an appointment time without calling. This provides 24/7 booking access while keeping your diary accurate and improving the patient experience.

- Automated reminders and confirmations: SMS and email reminders reduce missed appointments. Built-in reminders support clear physician-patient communication and help keep your schedule organised.

- Secure messaging tools: Electronic patient portals create a reliable way for clinics to respond to common questions. GDPR-compliant messaging systems support safe interactions and allow clinicians to provide visit summaries digitally.

- Digital forms and assessments: Smart forms allow patients to submit assessments before their visit, improving accuracy and saving time during face-to-face communication.

- Video consultations: A built-in video consultation platform allows clinicians to discuss care plans remotely, making it easier to maintain professional patient-clinician communication when face-to-face communication isn't possible.

These patient management system features work together to support both clinical efficiency and patient satisfaction. Collecting patient feedback through these digital tools helps improve the patient experience.
Final thoughts
Good physician-patient communication is a core part of quality care. By using clear language, listening attentively, and adapting your communication style, you create a more supportive patient experience.
Regularly reviewing your clinical communication and continuing to deliver patient-centered care helps build trust and supports better outcomes. How to build trust with patients starts with making communication a priority in everyday medical practice.
See how WriteUpp's tools help you simplify patient communication and improve outcomes without adding admin work.



Join over 50,000 clinicians that we've helped using WriteUpp
Start my free trial




.png)

.png)
.png)